The guidelines provided by the New York State Workers Compensation Board offer general principles for addressing Traumatic Brain Injury (TBI). These directives aim to assist healthcare professionals in determining appropriate strategies for managing individuals with traumatic brain injuries as part of a comprehensive care plan.
Healthcare practitioners specializing in Traumatic Brain Injury can rely on the guidance from the Workers Compensation Board to make well-informed decisions about the most suitable approaches for caring for and treating patients with TBI.
It is important to emphasize that these guidelines are not intended to replace clinical judgment or professional expertise. The ultimate decision regarding the management of Traumatic Brain Injury should involve collaboration between the patient and their healthcare provider.
Guiding Lights: Nurturing the Recovery Journey After Traumatic Brain Injury
In the realm of clinical practice, this guideline extends a caring hand to aid in the assessment and treatment of adults grappling with the aftermath of traumatic brain injury (TBI). Let’s navigate the key points:
- Decoding Traumatic Brain Injury (TBI): Unveiling the Definition
- TBI, a poignant chapter in the book of acquired brain injuries, unfolds when an abrupt trauma unfurls its impact on the delicate canvas of the brain.
- The narrative of trauma embraces diverse scenarios: a head encountering an object, a collision with an object, the brain experiencing an acceleration/deceleration sans direct external trauma, the intrusion of a foreign body into the brain, the repercussions of forces from events like blasts or explosions, and other impactful forces.
- Tiers of Impact: The Triad of TBI Acuity
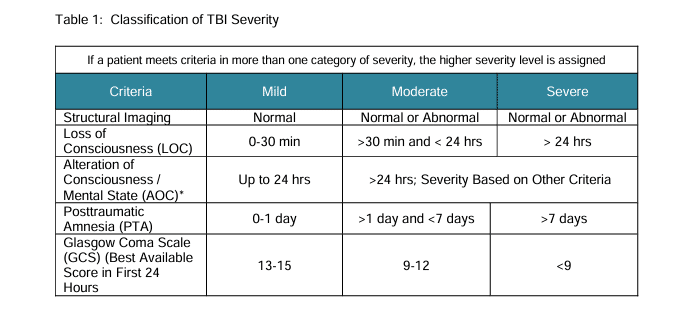
- TBI dons three distinct guises, each reflecting a different tier of severity: mild, moderate, and severe. The subtleties of this classification mirror the extent of the intricate damage woven into the fabric of the brain.
- The gentlest touch, known as mild TBI, wears the alias of a concussion, whispering of a trauma that, while impactful, leaves a lighter imprint.
- Glasgow Coma Scale: Illuminating Conscious Realms
- The guidelines enlist the aid of the Glasgow Coma Scale, a beacon in the neurological landscape. This scale, both an initiator and a companion in the journey, offers an objective measure to fathom the conscious state of an individual. It unfolds its significance not just in the initial encounter but in the ongoing odyssey of assessment.
In essence, this guideline is a compass for healthcare practitioners, illuminating the path to understanding and addressing the intricate challenges woven into the tapestry of traumatic brain injury.
Embarking on the journey through traumatic brain injury (TBI), each tier unfolds a unique chapter in the narrative, defining the contours of impact and recovery:
- Mild TBI – The Gentle Echo: Concussion
- In this nuanced realm, a tale is woven with at least one of the following threads:
- A gentle dance with consciousness, where either the person remained conscious or embraced a brief slumber of less than 30 minutes.
- Memory, a fleeting companion, left its trace for a span not exceeding 24 hours.
- The Glasgow Coma Scale (GCS) painted a portrait with hues ranging from 13 to 15, a testament to the resilience within.
- In this nuanced realm, a tale is woven with at least one of the following threads:
- Moderate TBI – The Pensive Pause: A Deeper Reverie
- The narrative takes a contemplative turn, embodying:
- A longer sojourn into unconscious realms, extending beyond 30 minutes and gracefully lingering up to 24 hours.
- The dance with memory, a more profound exchange, spanning from 24 hours to a week.
- GCS, the storyteller, narrates with scores donning the attire of nine to 12, encapsulating the profound impact etched within.
- The narrative takes a contemplative turn, embodying:
- Severe TBI – The Profound Odyssey: Beyond the Horizon
- Here, the journey plunges into depths:
- Unconsciousness stretches its wings, embracing a realm beyond 24 hours, where time becomes a fluid companion.
- Memory, an elusive wisp, lingers in the corridors of forgetfulness for more than a week.
- GCS, the silent narrator, whispers with scores that bow beneath eight, a reflection of the profound odyssey etched into the soul.
- Here, the journey plunges into depths:
In essence, this spectrum, ranging from mild echoes to profound odysseys, crafts a roadmap for understanding and navigating the varied landscapes within traumatic brain injury.
The Glasgow Coma Scale (GCS), a beacon in the realm of neurological evaluation, serves as a compass for discerning the intricate landscape of a person’s conscious state. Designed for both initial and subsequent assessments, the GCS stands as a stalwart method, offering a bedside tableau of conscious level impairment—the poignant clinical signature of acute brain injury.

In essence, the GCS functions as a neurological scale, unveiling the tapestry of consciousness through a meticulous examination. It not only captures the immediate impact but also becomes a guiding light in the ongoing journey of assessment, paving the way for a nuanced understanding of the evolving landscape of brain health.
Navigating the Aftermath: Understanding Traumatic Brain Injury (TBI)
When the delicate balance of the mind is disrupted by head trauma, it manifests in a spectrum of alterations to mental status. The aftermath may unfold with symptoms like a bewildered gaze, a sense of uncertainty, and a foggy comprehension of unfolding events. Confusion becomes a companion, clouding the ability to think clearly and respond appropriately to queries about one’s mental state. Describing events before or after the trauma becomes an arduous task, painting a vivid picture of the challenges that ensue.
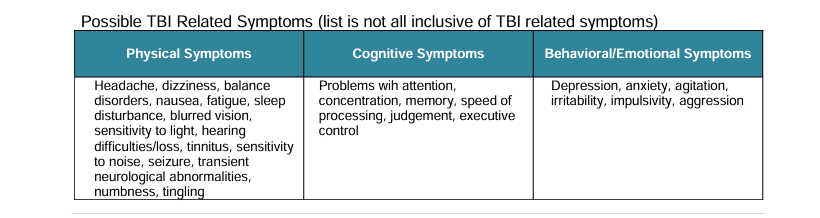
Traumatic Brain Injury (TBI) unfurls a tapestry of potential issues, both short and long-term. From cognitive functions like attention and memory to motor skills involving extremity weakness, TBI casts a wide net. Sensory realms may also bear the brunt, impacting hearing, vision, and perceptions of touch. The neurological landscape is not immune, giving rise to headaches, impaired coordination, balance issues, and the looming specter of seizures. Behaviors too may be reshaped, ushering in emotional regulation challenges, depression, anxiety, aggression, and alterations in behavioral control and personality.
Mild TBI, often synonymous with a concussion, typically charts a benign and self-limiting course. However, in a subset of cases, the symptoms persist, creating a unique landscape of challenges. While many experience resolution within days to a month, a fraction grapples with persistent symptoms extending beyond a year post-injury. These enduring symptoms encompass physical, cognitive, emotional, behavioral, and sleep-related facets, painting a nuanced portrait of the journey through the aftermath of a concussion.
Navigating the Aftermath: Understanding Post-Concussion Syndrome
Post-concussion syndrome (PCS) emerges as a term employed by many practitioners to encapsulate a persistence of symptoms extending beyond the typical recovery span post a concussion. Initially, common complaints encompass impaired memory, attention, and executive function, surfacing immediately after mild Traumatic Brain Injury (mTBI). For the majority, these symptoms relent within a few hours to days, marking a restorative trajectory. However, a subset of individuals recounts the emergence of new, persistent, or worsening cognitive symptoms, a phenomenon that may linger for weeks, months, or even years post-injury.
In understanding PCS, it’s crucial to recognize that those grappling with persistent symptoms might harbor pre-existing or co-existing conditions that influence the endurance of these symptoms. An inclusive evaluation and management approach must weigh these factors in the intricate landscape of post-concussive syndrome.
Traumatic Brain Injury (TBI) casts a long shadow, potentially leading to a lifetime of deficits. This underscores the importance of a comprehensive, long-term medical management strategy. Tailored management and treatment hinge on ongoing clinical evaluations, factoring in medical diagnoses, associated impairments, cognitive abilities, expected functional gains, and tangible progress evidenced by documented functional outcomes. The spectrum of management services spans from inpatient to outpatient rehabilitation and supportive living programs, contingent upon the severity of TBI and its associated impairments. In essence, the approach is a dynamic continuum, adapting to the unique needs and challenges posed by each individual’s TBI journey.
While these guidelines are typically written for care of patients in the ambulatory/outpatient setting, it is recognized that TBI carries with it an increased probability of patients requiring therapeutic interventions, typically delivered in the inpatient hospital setting, to be continued in other settings, such as long term care, community or outpatient rehabilitation, or even home care. These guidelines do not capture those interventions, and clinical decision-making regarding such interventions should be made on a case-by-case basis, based on the severity of the ongoing symptoms and the resultant type and magnitude of clinical needs, the complexity of which may require a multi-disciplinary approach.