Total hip arthroplasty dislocation is defined as complete loss of articulation of the hip joint after total hip replacement surgery. It means that the head of the femur has no contact with the cup inside the artificial hip joint.
This is unfortunately one of the most common causes of decreased patient satisfaction and reasons for a revision of hip after total hip replacement surgery.
Dr. Karkare was in the news for his expertise on the treatment of recurrent hip dislocation
When a dislocation happens, it means the bones will no longer be where they should be and should be treated it as an emergency. Medical attention is recommended as soon as possible because if it is left untreated, the dislocation could lead to damage of the surrounding blood vessels, nerves or ligaments.
The most common time this happens is first six to eight weeks after the index hip replacement surgery. There are two periods where the incidence of dislocation peaks after hip replacement surgery. The first time is in the immediate postoperative period within the first six to eight weeks of the surgery and the second peak is several years later. The causes of dislocation are different depending upon the time of dislocation after hip replacement surgery.
There are numerous mechanisms of total hip dislocation and the treatment mainly depends on the cause of the dislocation. As an example, malpositioning of the stem of the femoral component is responsible for early dislocations. If there is contact between the neck of the femur and the cup in the early range of motion, this can result in leverage of the femoral head out of the cup and is responsible for early to intermediate dislocations. The reason for the hip dislocating is that impingement can lever out the head and lead to separation of the head from the cup in the range of motion where the cup articulates with the femoral prosthesis within the physiological range of motion of the hip joint.
Contact between the untrimmed acetabular edges and femoral prosthesis could be another reason for impingement. This type of impingement is between bone and the stem and not between the acetabular prosthesis and the femur.
Hyperlaxity of a joint due to muscular insufficiency or lack of soft tissues is perceived as a cause of dislocation and is attributed to the soft tissues that the patient has and is also an early cause of total hip dislocation.
Dislocation can also be classified according to the direction in which the femoral head dislocates. The head can be dislocated anteriorly ( the front of the hip) or posteriorly (behind the hip) superiorly (above the hip joint) and also it could be dislocated inferiorly (below the hip joint). The posterior hip dislocation is most common after posterior hip arthroplasty. Anterior hip dislocation is typically a consequence of anterior hip replacement surgery. The head can be dislocated superiorly both after anterior and posterior approach. The inferior dislocation of the hip is typically traumatic and is consequence of high energy injury. It is uncommon after joint replacement surgery, I have not encountered inferior hip dislocation after total hip replacement surgery and is extremely rare.
I classify treatment in two types; one is closed reduction of the hip, which is done in the acute stage immediately after dislocation. The procedure is to place the head of the femur back into the cup so that the patient can immediately stand and can walk after the procedure. For a “regular” hip replacement this maneuver is done in the emergency room and the patient is completely anesthetized for the procedure.
If the surgeon cannot reduce the dislocation in the emergency room, the patient has to be taken to the operating room for a closed reduction under complete anesthesia. The most common reason for not getting a reduction in the emergency room is inadequate muscle relaxation. Inadequate muscle relaxation can happen because the ER physician is unable to give enough relaxation medication to the patient for the procedure to be performed safely in the emergency room. Unless the dislocation is chronic (which means that the dislocation has been present for a very long time), it is generally possible to do a closed reduction in the operating room.
The second type of treatment is surgical treatment, which is done when the dislocation is “recurrent”. I define recurrent dislocation as dislocation of the hip that happens more than three times. If the hip dislocates more than three times, then dislocation is going to continue unless the hip is surgically treated.
Schedule an Appointment Now
This “three-strike” rule (hip dislocating three times) for surgical intervention applies only to a hip that is “primary” hip (which means that the patient has had a regular head and a regular cup in the hip replacement). If the patient has had a constrained prosthesis, which is a prosthesis done for dislocating hip in the first place and if the patient then dislocates the hip that has a constrained prosthesis, it is extremely difficult to do a closed reduction in the emergency room or in the operating room. If a constrained line dislocates, the patient needs surgical intervention for reducing the dislocation and to prevent dislocation happening subsequently.
When surgical intervention is indicated, the most important consideration is to address the reason why the dislocation happened in the first place. I classify the reasons as “patient-related” factors, “surgeon-related” factors as well as “implant-related” factors.
There are numerous “patient-related” factors that predispose patients to dislocating their hip. There are several neuromuscular conditions place the patients at increased risk of dislocating their hip. Neuromuscular conditions including Parkinson’s Disease predispose patients to hip dislocation. Patients who have dementia have difficulty following hip dislocation precautions and are at increased risk. Patients who are at increased risk of fall are also at increased risk of dislocating the hip joints.
Noncompliant patients do not follow hip dislocation precautions. The noncompliance could be because of dementia, because of alcohol intake etc. Patients who have congenital hip dysplasia and certain metabolic bone disorders are also at increased risk of dislocation. Patients who undergo a revision hip replacement surgery, have a significantly increased risk of dislocating their hip joint.
There are some “surgeon-related” factors, which can lead to hip dislocation. If the surgeon does not accurately positioned the inclination of the acetabular and femoral component in the pelvis while doing the surgery, the hip can dislocate. Additionally, if the “off-set” of the hip (the horizontal distance from the center of the hip to the center of the stem) is not restored, the soft tissues are not balanced, the muscles are lax and the hip can therefore dislocate.
The surgeon’s surgical approach is also important. Studies have shown that certain surgical approaches are at increased risk of dislocation. Lastly and most importantly, the experience of the surgeon, the volume that the surgeon does, the surgical training of the surgeon is extremely important factor for the total hip arthroplasty to have an optimal outcome. I feel that the patient should undergo joint replacement surgery only by a surgeon fellowship-trained in hip and knee replacement surgery who does joint replacement surgery on a regular basis.
Lastly, there are “implant-related” factors which can lead to hip dislocation. There are certain hip stems that are “round” instead of “tapering” and do not allow good range of motion at the hip joint. Such stem geometries can cause impingement and lever out the femoral head leading to dislocation. Additionally, larger femoral heads are used to increase the jump distance and to decrease the risk of dislocation.
There is a certain compromise by increasing the size of the head because that can mean that the size of the polyethylene in the hip is thinner and the thinner polyethylene especially in a larger patient can have accelerated rate of wear. The hip dislocations that occur late after joint replacement surgery could be due to accelerated weight loss of the patient, which is correlated with increased risk of dislocation, correlated with late increased risk of dislocation. Additionally, if the plastic wears off the hip can become unstable leading to the head of the femur sliding out of the cup causing a dislocation.
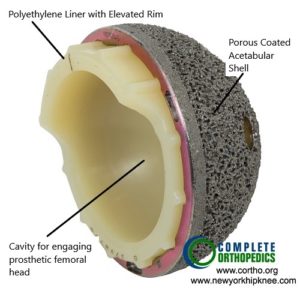
Polyethylene liner with an elevated rim
The image shows a polyethylene liner with an elevated rim to prevent the head from levering out of the socket.
For a patient with recurrent dislocation I start by evaluating the X-rays. I start with a low AP x-ray of the pelvis with the hip and also lateral of the affected hip. I also get CAT scan done for evaluation of the anteversion (inclination) of the femur and acetabulum. In the AP x-ray I look at the inclination of the cup, the off-set, the stability of the interface between femur and bone as well as stability of the interface between the cup and the bone. I also look at any limb length discrepancy in the AP x-ray.
In the lateral x-ray I get an assessment of the inclination of the cup as well as of the stability of the components. A CT scan is a very accurate way to measure the version (inclination) of the cup and to compare the version of the components to the contralateral side. If the CT scan shows accurate placement of all components with no issues with the off-set and a stable interface, I operate using a constrained liner.
I my preferred choice of a constrained cup where the locking mechanism of the liner to the cup is extremely stable. If there is malposition of the components, I correct the malposition of the components. Additionally, I increase the off-set and also make sure that there is no limb length discrepancy. For patients who are noncompliant, the options include use of a constrained liner or tripolar cup.
Total hip arthroplasty dislocation is complete loss of articulation between the head of the femur and cup and is a very frustrating complication following total hip arthroplasty. It is extremely important to be cognizant of patient factors that can lead to dislocation, the surgeon has to be competent to ensure that the components are accurately and correctly positioned and the right implants are used. If all precautions are followed, the hip dislocation risk can be significantly reduced.
Hip Dislocation Case Study
A 55-year-old male who came to us complaining of recurrent right hip prosthesis dislocation. He states stated that this had been occurring since he had a right Total Hip Arthroplasty (THA) a few years ago done at an outside institution, and he was in severe pain and discomfort…
Why choose Dr. Karkare?
As a top joint replacement specialist in New York City, Dr. Karkare has a stellar reputation, extensive experience, ensuring patients have the broadest array of safe and effective treatment options to relieve pain and other symptoms.

This enables every patient to make an informed, educated decision so they can feel confident in their care every step of the way.
To schedule your evaluation, call (516) 735-4032 or use our online contact form to learn more.
How Can I Help You?


