The guidelines provided by the New York State Workers Compensation Board are intended to assist healthcare professionals in evaluating Hip Osteonecrosis. These directives aim to support physicians and healthcare practitioners in determining the appropriate treatment for this condition.
Healthcare professionals specializing in Hip Osteonecrosis can rely on the guidance provided by the Workers Compensation Board to make well-informed decisions about the most suitable level of care for their patients.
It is crucial to emphasize that these guidelines are not intended to replace clinical judgment or professional expertise. The ultimate decision regarding care should involve collaboration between the patient and their healthcare provider.
Related Terms
Osteonecrosis • Avascular Necrosis (AVN) • Aseptic Necrosis • Ischemic Bone Necrosis • Ischemic Bone Death
Introduction
Osteonecrosis, also known as avascular necrosis, is a condition characterized by bone death. Some instances are categorized as occupational disorders, particularly in the context of dysbarism, which involves atmospheric compression/decompression. Workers such as divers and those in compressed air atmospheres may experience impaired blood supply to the femur due to nitrogen gas in the blood during excessively rapid decompression. Another reported cause is major trauma, where significant, discrete trauma is considered a risk factor.
However, the role of nontraumatic job-related physical factors is a subject of controversy. Treatment primarily focuses on mitigating the exposures believed to be responsible. Surgical procedures like “coring,” vascularized and unvascularized bone grafting, and osteotomy are occasionally employed. In severe cases, arthroplasty may be necessary.
Diagnostic Studies
initial assessment
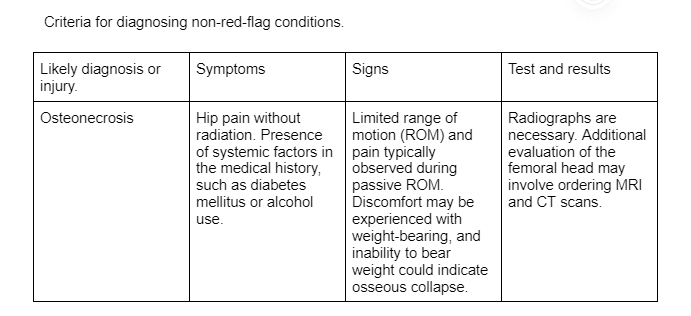
The initial assessment of hip disorders typically relies on a comprehensive approach involving history, physical examination, and radiographs. To ensure a thorough evaluation, the review of systems and examinations should extend beyond the hip to encompass the knee, spine, abdomen, and genitourinary tract. Imaging studies are often effective in diagnosing osteonecrosis, with radiographs being a common initial step.
If the cause of hip pain remains unclear after radiographs, magnetic resonance imaging (MRI) is generally the preferred imaging modality, with or without the use of gadolinium and other contrast agents. The criteria outlined below provide an overview of the clinical thought process for evaluating hip osteonecrosis.
Bone Scanning with SPECT
Suggested – Consider bone scanning with SPECT in selected cases of acute, subacute, or chronic pain to aid in diagnosing osteonecrosis and other conditions with increased polyosthotic bone metabolism, especially when evaluating more than one joint is necessary.
Indication/Rationale: Bone scanning proves beneficial in identifying areas of heightened bone metabolism, primarily serving its purpose in cases of osteonecrosis. Frequency/Dose/Duration: Typically, one evaluation is recommended. Evidence supporting the use of bone scans.
CT for Evaluating Osteonecrosis
Suggested – Opt for CT in evaluating patients with osteonecrosis, particularly when advanced imaging is necessary, but there are contraindications for MRI or when helical CT is not available.
Indications: This is suitable for cases of hip pain suspected to be from osteonecrosis but with contraindications for MRI.
Frequency/Dose/Duration: Generally, one evaluation is sufficient. A second evaluation may be needed in the presence of a significant clinical change or to assess progress/resolution.
Reasoning: While there is no clear preference of CT over MRI for osteonecrosis, CT is considered superior to MRI for imaging most hip abnormalities requiring advanced imaging of calcified structures. Helical CT is generally preferred over CT, but its use may be limited, especially in settings without helical CT.
Helical CT for Evaluating Osteonecrosis
Suggested – Consider helical CT for evaluating patients with osteonecrosis, especially in cases where there are contraindications for MRI.
Indications: This is suitable for instances of hip pain suspected to be from osteonecrosis, particularly when concerns about fracturing and collapse exist. It is also indicated for those requiring osteonecrosis evaluation but with contraindications for MRI.
Frequency/Dose/Duration: Generally, one evaluation is recommended. A second evaluation may be necessary in the presence of a significant clinical change or to assess progress/resolution.
Reasoning: Helical CT is deemed superior to MRI for imaging most hip abnormalities requiring advanced imaging of calcified structures. Although there is no clear preference of CT over MRI for osteonecrosis, helical CT is considered better at identifying fracturing and is recommended for select use. Evidence supporting the use of helical CT.
MRI for Diagnosing Osteonecrosis
Suggested – Opt for MRI in cases of subacute or chronic hip pain suspected to be due to osteonecrosis, especially when the diagnosis is unclear or if additional diagnostic evaluation and/or staging is needed.
Frequency/Dose/Duration: Typically, one evaluation is sufficient. A second evaluation may be required in the presence of a significant clinical change or to assess progress/resolution.
Reasoning: Helical computerized tomography is considered superior to MRI for imaging bone collapse. MRI, on the other hand, is considered superior for imaging bone marrow edema, which is inversely correlated with prognosis. Therefore, both tests offer distinct advantages.
X-Rays for Diagnosing Osteonecrosis
Suggested – Use x-rays for diagnosing osteonecrosis in all patients suspected to have this condition.
Frequency/Dose/Duration: Periodic x-rays to monitor the disease’s progression are a standard practice.
Reasoning: X-rays are valuable in evaluating most patients experiencing hip pain, aiding in both diagnosis and differential diagnostic considerations. In the early stages of osteonecrosis, x-rays may appear normal or show slight osteopenia, necessitating a high index of suspicion. Evidence supporting the use of x-rays/radiographs.
Ultrasound for Osteonecrosis
Not Recommended – Avoid using ultrasound for diagnosing osteonecrosis.
Medications
For the majority of patients, ibuprofen, naproxen, or other older generation NSAIDs are recommended as the first-line medications. Acetaminophen (or the analog paracetamol) may be a reasonable alternative to NSAIDs for patients who are not suitable candidates for NSAIDs, although most evidence suggests acetaminophen is modestly less effective. There is evidence indicating that NSAIDs are as effective for relieving pain as opioids (including tramadol) and have less impairment.
Non-Steroidal Anti-inflammatory Drugs (NSAIDs) for Treatment of Acute, Subacute, or Chronic Osteonecrosis
Recommended – Use NSAIDs for the treatment of acute, subacute, or chronic osteonecrosis.
Indications: NSAIDs are recommended for the treatment of acute, subacute, or chronic osteonecrosis, with over-the-counter (OTC) agents being a reasonable first-line option.
Frequency/Duration: As-needed use may be reasonable for many patients. Indications for Discontinuation:
Discontinue NSAIDs in case of resolution of osteonecrosis, lack of efficacy, or the development of adverse effects necessitating discontinuation.
NSAIDs for Patients at High Risk of Gastrointestinal Bleeding
Recommended – Use NSAIDs in conjunction with cytoprotective classes of drugs, such as misoprostol, sucralfate, histamine Type 2 receptor blockers, and proton pump inhibitors, for patients at high risk of gastrointestinal bleeding.
Indications: Consider cytoprotective medications for patients with a high-risk factor profile who also have indications for NSAIDs, especially if longer-term treatment is contemplated. At-risk patients include those with a history of prior gastrointestinal bleeding, the elderly, diabetics, and cigarette smokers.
Frequency/Dose/Duration: Recommended cytoprotective medications include proton pump inhibitors, misoprostol, sucralfate, and H2 blockers, with dosages and frequencies per the manufacturer’s recommendations. There is generally no substantial belief in differences in efficacy for preventing gastrointestinal bleeding.
NSAIDs for Patients at Risk for Cardiovascular Adverse Effects
Patients with known cardiovascular disease or multiple risk factors for cardiovascular disease should engage in a discussion regarding the risks and benefits of NSAID therapy for pain.
Recommended – Acetaminophen or aspirin is considered the safest first-line therapy with regards to cardiovascular adverse effects.
Recommended – If necessary, non-selective NSAIDs are preferred over COX-2 specific drugs. For patients taking low-dose aspirin for primary or secondary cardiovascular disease prevention, to minimize the potential for the NSAID to counteract the beneficial effects of aspirin, the NSAID should be taken at least 30 minutes after or 8 hours before the daily aspirin.
Acetaminophen for Treatment of Osteonecrosis Pain
Recommended – Use acetaminophen for the treatment of osteonecrosis pain, especially in patients with contraindications for NSAIDs. Indications: All patients with osteonecrosis pain, including acute, subacute, chronic, and post-operative.
Dose/Frequency: Follow the manufacturer’s recommendations and may be utilized on an as-needed basis. There is evidence of hepatic toxicity when exceeding four grams per day.
Indications for Discontinuation: Discontinue in case of resolution of pain, adverse effects, or intolerance.
Opioids
Recommended – for limited use, with a maximum duration of seven days, as adjunctive therapy for NSAIDs. Indications – Pain management, where a brief prescription of opioids is considered as an adjunct to more efficacious treatments, especially NSAIDs and acetaminophen. This is particularly relevant for achieving nocturnal pain relief.
Frequency/Duration – Prescribed as needed throughout the day initially, and later only at night before gradually tapering off. Rationale for Recommendation – In cases where patients experience insufficient pain relief with NSAIDs, judicious use of opioids may be considered, primarily for nocturnal use to facilitate sleep. Opioids are recommended for brief, selective use.
Bisphosphonates
Not Recommended – for the treatment of osteonecrosis.
Anti-Convulsant Agents (including Topiramate)
Not Recommended – for the treatment of pain associated with osteonecrosis.
Gabapentin and Pregabalin
Not Recommended – for pain associated with osteonecrosis.
Glucocorticosteroids
Not Recommended – for the treatment of osteonecrosis.
Treatments
The initial approach to treating mild to moderate cases of osteonecrosis is to identify and address reversible risk factors. This involves reducing or eliminating activities that provoke symptoms, including avoiding dysbaric exposures. In cases of moderately severe or severe osteonecrosis, prompt surgical intervention is typically recommended, especially if collapse has occurred.
Assessing the severity of the disease is the first step in the evaluation of osteonecrosis. Early intervention involves the elimination of decompression atmospheres, with a focus on avoiding activities that significantly worsen symptoms. Nonprescription analgesics may be sufficient for pain relief in most patients with hip pain from osteonecrosis. However, if the condition is progressing or the severity is advanced, surgical intervention becomes necessary.
For acute and subacute cases of osteonecrosis, avoiding de/compression atmospheres is crucial. Patients with osteonecrosis should refrain from undergoing any de/compression atmospheres until the condition is resolved. Activities involving high force or impact (e.g., jumping) should generally be avoided in patients with osteonecrosis, especially those with more severe disease at risk of collapse, until substantial improvement or resolution occurs. Regardless of the phase of osteonecrosis (acute, subacute, chronic), adherence to decompression tables is highly advisable.
Surgery
Core decompression surgery is recommended for the treatment of osteonecrosis in patients with generally moderate to severe cases who are not responding to risk factor modification or are considered at risk of collapse. This intervention is advised when further delay in treating risk factors or employing hyperbaric oxygen is deemed too risky.
Arthroplasty is recommended for the treatment of osteonecrosis with collapse or severe disease unresponsive to non-operative treatment. Patients with collapse of the femoral head are immediate candidates for arthroplasty. Additionally, individuals with severe osteonecrosis who do not respond to risk factor modification or are considered at risk of immediate collapse are also candidates for arthroplasty. The rationale behind this recommendation is that once the head of the femur collapses, arthroplasty is usually the appropriate treatment.
Other Treatments
To address osteonecrosis and its associated risks, it is recommended to reduce or eliminate activities that pose significant risks for the condition, including the avoidance of dysbaric exposures.
Non-weight bearing activities are not recommended for patients with osteonecrosis.
Hyperbaric oxygen (HBO) therapy is recommended for the treatment of osteonecrosis, particularly in Ficat Stage 2. It may be reasonable to attempt HBO in patients with more severe osteonecrosis. The recommended frequency, dose, and duration include up to 30 treatments. Indications for discontinuation include completing the course, intolerance, clinical resolution, or osteonecrosis collapse.

